Dear All,
I wish to pose a question to HIFA2015 members as it is still a big concern to me. How can we ensure that health information is utilized at the point of generation for evidence based decision making to improve the quality of care in our health care systems particularly in developing countries? In Kenya, scenarios of a patient being sent to pharmacy for drugs after being seen by the clinician and a prescription is written, only to find that the drugs are out of stock, is common. This is common at the public hospitals. If only the information on the drugs available was circulated to different clinicians seeing the patients by the beginning of the day, the patient would have saved a lot of suffering queuing for drugs only to be disappointed that they are not available. Clinicians will only prescribe for the available drugs if they had the information. This has its impact on the quality of care and also on services offered to our clients especially in the public hospitals.
Beatrice Muraguri HIFA2015 profile: Beatrice Muraguri is Health Information Officer with the Ministry of Health, Nairobi, Kenya.
MAY I add that the same scenario exists in Nigerian hospitals and patients and their relatives sometimes have to visit several pharmacies at huge expense, stress and waste of valuable time to buy medications or equipment. Why? Especially when each hospital can determine what drugs are in stock, are low in stock and finished thereby requiring replacement.
I have now sent our Chief Pharmacist at the National Hospital, Abuja, a list of the common drugs I might require in Neurosurgery for procurement. I know what drugs I need , they know what drugs my patients are likely to require, so hopefully we will get it right.
Comments and opinions please.
Biodun Ogungbo
Monday 14 December 2009
Sunday 13 December 2009
Friday 13 November 2009
trauma care in abuja: a time to wake up
the management of trauma patients in abuja is appalling. there is a complete lack of understanding of the concepts of advanced trauma life support. even the tenets of basic life support are not applied in patient management. many trauma patients are simply not reviewed not treated and turned away, sent to the nearest big general hospital without proper management. and many die on the way in hearses otherwise called ambulances. they are really better called 'taxis'. some hospitals actually use taxis or even relatives cars to send patients between facilities. this is wholly not acceptable. we must work together to preserve life at every step.
what we need to do? we need to work together. its really simple. resuscitate the patient. sort out any problems with airway, breathing and blood pressure. put in an intravenous line or two and put up fluids. if hypotensive give a plasma expander. stop any immediate accessible bleeding. investigate in trauma as much as you can safely. get a skull x-ray, cervical x-ray and chest or long bone x-rays as necessary. get as much information as you can and then transfer. let the other hospital have as much information as possible so they know where to start from in continuing the care of the patient.
resuscitate: investigate: transfer. Simple
Saturday 24 October 2009
On the issue of burr holes done by general surgeons
Since having some interaction with general surgeons who have on occasion had to manage patients with head injury in Abuja, I have come to realise that there is more to this than meets the eye.
Many of the surgical interventions are actually unnecessary and frankly dangerous with more harm than good being done. The interventions are often inadequate and increase the morbidity and mortality for the patient. I wont advocate for a stop to the performance of such procedures but I will insist that anyone hoping to perform such procedures must be properly informed, educated and taught how to do it before embarking on this. At least in Abuja. I cannot influence what happens elsewhere.
The key problem at first glance is 'wrong' diagnosis. It is imperative to relate the clinical history and the clinical examination to the imaging. All three: history, examination and imaging results must tally. The diagnosis must be correct. The importance of any imaging feature must be interpreted in the line of the patients clinical presentation and the condition. There have been patients in good clinical condition and those in extremis who have had burr hole performed unnecessarily. In those cases who were going to die anyway, it was a waste of time and resources, BUT in those who were good grade patients, it led to increase morbidity and eventual mortality. A real waste of life.
The problem I have seen in a few cases is the radiological diagnosis. The radiologists report what they see. They often fail to relate it to the clinical condition of the patient. Often in acute cases, the reporting radiologist was not actually there when the patient was being scanned and is reporting the scan hours later. Its not their job to then prescribe treatment or advice on such an issue.
Let me give you an example. Young woman with mild to moderate head injury.. gcs 12 to 13/15. Scan reported as showing an acute subdural hematoma. Surgeon decides to offer burr hole to remove subdural. Patient then had to be ventilated in ITU post operatively. Patient died of complications of treatment: surgical and anaesthetic. I review scan and note a thin film of subdural.... not surgical..... no need to have had a burr hole.... maybe patient may still be alive if left alone?? The radiologist did not inform about size of the clot and its significance just that there is a subdural clot. Surgeon did not relate size to clinical condition of the patient.
Another example. Young man with head injury..gcs 3/15 right from the start. Intubated for a scan which shows an acute subdural clot and temporal lobe contusions. Surgeon offers burr hole drainage of the subdural. Patient died in ITU days later. I review the scan and note a small film of subdural but more important significant lobar contusions. Patient may have benefited from a decompressive craniectomy and removal of the contusions if anything needed to be done. I actually would not have offered any intervention given the poor clinical state at presentation. Radiologist did not emphasise the small subdural and the more important contusions. Surgeon failed to appreciate what was really important in the clinical presentation and imaging.
May I finish this diatribe by saying categorically, that burr holes are for chronic subdural collections only. They cannot be used to treat an acute extradural hematoma, an acute subdural hematoma or an intracerebral hematoma especially in untrained hands.
The teaching of general surgeons will commence in Abuja in earnest working with these basic principles: Know the patient, read the scan, discuss with the radiologist and then ask advice of a neurosurgeon before making any attempts at a burr hole drainage. Do burr hole ONLY for a chronic subdural hematoma or perhaps for a brain abscess. Burr holes cannot treat an acute subdural or an extradural hematoma. Certainly not with a Ghajar guide.
Many of the surgical interventions are actually unnecessary and frankly dangerous with more harm than good being done. The interventions are often inadequate and increase the morbidity and mortality for the patient. I wont advocate for a stop to the performance of such procedures but I will insist that anyone hoping to perform such procedures must be properly informed, educated and taught how to do it before embarking on this. At least in Abuja. I cannot influence what happens elsewhere.
The key problem at first glance is 'wrong' diagnosis. It is imperative to relate the clinical history and the clinical examination to the imaging. All three: history, examination and imaging results must tally. The diagnosis must be correct. The importance of any imaging feature must be interpreted in the line of the patients clinical presentation and the condition. There have been patients in good clinical condition and those in extremis who have had burr hole performed unnecessarily. In those cases who were going to die anyway, it was a waste of time and resources, BUT in those who were good grade patients, it led to increase morbidity and eventual mortality. A real waste of life.
The problem I have seen in a few cases is the radiological diagnosis. The radiologists report what they see. They often fail to relate it to the clinical condition of the patient. Often in acute cases, the reporting radiologist was not actually there when the patient was being scanned and is reporting the scan hours later. Its not their job to then prescribe treatment or advice on such an issue.
Let me give you an example. Young woman with mild to moderate head injury.. gcs 12 to 13/15. Scan reported as showing an acute subdural hematoma. Surgeon decides to offer burr hole to remove subdural. Patient then had to be ventilated in ITU post operatively. Patient died of complications of treatment: surgical and anaesthetic. I review scan and note a thin film of subdural.... not surgical..... no need to have had a burr hole.... maybe patient may still be alive if left alone?? The radiologist did not inform about size of the clot and its significance just that there is a subdural clot. Surgeon did not relate size to clinical condition of the patient.
Another example. Young man with head injury..gcs 3/15 right from the start. Intubated for a scan which shows an acute subdural clot and temporal lobe contusions. Surgeon offers burr hole drainage of the subdural. Patient died in ITU days later. I review the scan and note a small film of subdural but more important significant lobar contusions. Patient may have benefited from a decompressive craniectomy and removal of the contusions if anything needed to be done. I actually would not have offered any intervention given the poor clinical state at presentation. Radiologist did not emphasise the small subdural and the more important contusions. Surgeon failed to appreciate what was really important in the clinical presentation and imaging.
May I finish this diatribe by saying categorically, that burr holes are for chronic subdural collections only. They cannot be used to treat an acute extradural hematoma, an acute subdural hematoma or an intracerebral hematoma especially in untrained hands.
The teaching of general surgeons will commence in Abuja in earnest working with these basic principles: Know the patient, read the scan, discuss with the radiologist and then ask advice of a neurosurgeon before making any attempts at a burr hole drainage. Do burr hole ONLY for a chronic subdural hematoma or perhaps for a brain abscess. Burr holes cannot treat an acute subdural or an extradural hematoma. Certainly not with a Ghajar guide.
Sunday 4 October 2009
poverty is a big issue
The one thing that is creating a problem at the moment is poverty and the inability of some patients to afford the costs of investigations and treatment. Radiology especially CT and MRI scans are expensive and surgical treatment is also very expensive for many. Real patients with real problems and significant risks of increased morbidity and mortality are seen without ability to pay for treatment. It saddens.
What can we do and how can one help? How many free treatments can one afford to give out before you stop being able to help even anyone? What ways can we device to help? Because we do have to do something. And fast.
First, we perhaps should encourage the development of charities, the involvement of charities in care and establish specific foundations and endowments to fund some investigations and operations. We should also perhaps encourage and set up support groups for conditions such as stroke, tumours and trauma. The charities and groups could seriously help to inform, educate and generate much needed funds for particular projects.
Involving well meaning members of the public in specific projects for hospital development and endowments is important and should be actively encouraged. All hands need to be on deck especially in preventive measures to reduce the incidence of many conditions. We need to actively educate doctors and nurses and then the general public on ways to prevent some preventable diseases.
What can we do and how can one help? How many free treatments can one afford to give out before you stop being able to help even anyone? What ways can we device to help? Because we do have to do something. And fast.
First, we perhaps should encourage the development of charities, the involvement of charities in care and establish specific foundations and endowments to fund some investigations and operations. We should also perhaps encourage and set up support groups for conditions such as stroke, tumours and trauma. The charities and groups could seriously help to inform, educate and generate much needed funds for particular projects.
Involving well meaning members of the public in specific projects for hospital development and endowments is important and should be actively encouraged. All hands need to be on deck especially in preventive measures to reduce the incidence of many conditions. We need to actively educate doctors and nurses and then the general public on ways to prevent some preventable diseases.
Wednesday 9 September 2009
What do you think? Can we find sponsors to buy these?


This is open to discussion, thoughts and opinions.
Neurosurgical Equipment Presented by the World Federation of Neurosurgical Societies' Foundation
Neurosurgical Equipment Presented by the World Federation of Neurosurgical Societies' Foundation
With this Basic Set of Neurosurgical Instruments, WFNS, together with Aesculap, has initiated a worldwide project. It provides an attractive platform for sponsoring adequate neurosurgical instruments in countries that are in great need of such equipment.
This set of instruments can be used for the most common neurosurgical procedures. We hope to find numerous sponsors who will purchase this Basic Set of Neurosurgical Instruments and thereby support physicians in economically challenged countries who are devoted to neurosurgery and neurosurgical patients.
Professor Temitayo Shokunbi (Ibadan) has done a lot in getting many of these basic sets for different hospitals in Nigeria. It is important for all neurosurgeons to actively find sponsors and identify hospitals in which these basic sets would be of real advantage and save lives.
Along with the Basic Set of Neurosurgical Instruments, the WFNS Foundation also provides basic neurosurgical training for general surgeons who must render such services in developing countries. I think we should also start training general surgeons in basic neurosurgery; they already attempt procedures especially simple burrholes and just require some hands on experience to be better; second, teaching the young surgeons may stimulate some to take up neurosurgical training.
Biodun
Tuesday 8 September 2009



I was over at IMPLANTS INTERNATIONAL office and factory this afternoon. This is a company based in Thornaby, on Teeside, in the United Kingdom, manufacturing implants related to trauma, orthopedics and spine. The range of products is wide and the expertise/ quality of the products cmparable to any other big players in the field. Some of the products especially related to spine and neurosurgery are as shown: anterior cervical plates, artificial cervical discs, cages and lateral mass screws. Further, the company manufactures pedicle screw fixation screws and implants for most joints in the body.
I was well impressed and pleasantly surprised by what I saw.
The key information is that the company can support and supply all we might need to manage our patients with degenerative and traumatic spinal lesions. The company has a wide range of products from cervical to sacrum and prosthesis for joint replacements.
Its exciting times ahead with the possibility and the ablity to offer our patients comprehensive and affordable surgery obviating the need to travel to India, South Africa or even Britain for quality care. We can now do all the operations locally and increase our acceptance by a sceptical Nigerian public.
I am particularly looking forward to working with this company and Drs, Opadele, Nasiru and Adeolu in providing a comprehensive spine service in Abuja.
Saturday 5 September 2009
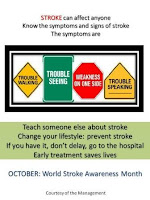
stroke information for OCTOBER stroke awareness month
 Stroke
StrokeStroke is the acute and dramatic interruption of the blood supply to the brain or hemorrhage into brain tissue. Stroke is now an important and a leading cause of death in most countries. In America, approximately 500,000 strokes occur each year. The estimate for Nigeria is around 200,000. Of these about 70% die within a year and the rest are often disabled. Stroke causes significant disability and death in many countries and places a huge financial burden on health services. This is estimated at £2.318 billion costs to the National Health Service in the United Kingdom for 1995-6 alone. In Nigeria, the impact on the local economy and the financial burden of stroke has not been estimated. The costs are both physical and material; the social effects often devastating. Costs are often borne by individuals and families.
Can you afford to have a stroke?
Stroke is a major life changing event. It is sudden, happens out of the blue and brings about unexpected changes. It can lead immediately to death or permanent disability. The effect on the individual and the family can be long lasting. Many stroke patients die or suffer untold misery. Stroke can blight even the most resourceful family and bring untold misery with possible financial ruin. Many families are decimated due to stroke with the loss of a bread winner. Even if a breadwinner still exists within the family unit, the resources are expended on the sick relative.
No two strokes are the same and the experience is individual. Nobody else can understand the impact on an individual or a family. For the individual nobody else knows what it is like for YOU to have had a stroke. The effects can be mild, minor or devastating. The disability can range from or be a combination of different deformities and disabilities. These could include blindness, confusion and mental incapability, loss of speech and use of language, depression, loss of identity, anxiety, helplessness, loss of a limb with functional disability, dependency, sleeplessness, loss of control and dignity. The high social and economic burden of stroke, on individuals, families, societies and the nation, calls for effective strategies for prevention, treatment, and rehabilitation. Currently, in Nigeria, there is little or no support for stroke victims and the poor medical infrastructure is unable to provide effective rehabilitation. Prevention is therefore very important.
What you need to know about stroke?
Remember the symptoms of a stroke are sudden weakness of an arm or a leg, difficulty with speech, problems with walking, sudden blindness in one eye, confusion and headache. The symptoms can be short lived, they can come and go: each episode lasting for minutes to hours or a day (transient ischemic attack: called T.I.A. or mini stroke). If you or a relative has any of these symptoms, you need to react FAST. Do not hesitate. Do not ignore this type of symptoms as they may herald a bigger stroke which could become permanent and devastating. "Brain attack!" is a term used to describe the acute presentation of stroke, which emphasizes the need for urgent action. The concept of "brain attack" is very important to sensitize physicians and the public to the need for rapid mobilization and early treatment of stroke patients. This approach of treating stroke as an emergency requires educational programs directed at the general public, general practitioners, and primary and emergency department physicians. It helps to teach the early recognition of stroke symptoms and the importance of treating stroke with the same urgency as for heart attack. The longer the delay before active and effective therapy, the more brain tissue is lost by the patient. Remember the saying, 'time is brain'. If you waste time and delay in getting effective help, you lose brain. It has been estimated that someone whose brain is starved of oxygen for an hour ages by 3.5 years.
Most basic studies show that to be effective, acute intervention to restore blood to the brain must take place within a few hours. Damaged brain and the surrounding 'at risk' brain need to be protected as soon as possible. Doctors have a duty to evaluate a stroke patient rapidly, investigate astutely and prescribe effective medication within 1-3 hours of the event or within the first hour of arrival in hospital. Most people do not present to the doctor in time and this delay could be very costly. Many ignore the early warning signs of stroke. Do not go to bed and hope it will go away by the time you wake up. You may not wake up. Act FAST, if you think someone may be suffering a stroke.
What is FAST?
FAST requires an assessment of three specific symptoms of stroke:
Facial weakness - can the person smile? Has their mouth or eye drooped?
Arm weakness - can the person raise both arms? Is one arm or leg weak?
Speech problems - can the person speak clearly and understand what you say?
Time to call or go straight to the hospital. If the person has failed any one of these 3 tests written above, you must act fast. Stroke is a medical emergency. Do not delay. Ensure that it is investigated by a competent doctor. This is vital information. Do not ignore it even if the symptoms resolve. This can happen and it's called Transient Ischemic Attack or TIA for short. This is actually a warning sign of an impending major stroke. This is the time to take action to prevent stroke. Getting help early may prevent a further stroke or lessen brain damage thereby limiting its effects on the person. About a third of patients with a TIA suffer a major stroke in the near future. Note that the symptoms are similar to a stroke but wear off within 24 hours and sometimes in minutes. Temporary blind spots or a curtain covering the vision, difficulty in talking, numbness, tingling or weakness of the face or down one side of the body are all signs of TIA. Many strokes can be prevented by heeding the warning signs and treating underlying risk factors.
The types of stroke
There are three types of stroke and hundreds of different underlying causes. The three types are called ischemic stroke, haemorrhagic stroke and subarachnoid haemorrhage. Strokes are either due to obstruction of the blood supply to a part of the brain or rupture of the blood vessel leading to a blood clot forming within the brain. It can be devastating as discussed earlier.
What can you do to prevent a stroke?
Life style modification is the key preventive strategy to prevent stroke. Be aware of the various risk behaviours that can lead to someone developing a stroke. These are bad habits such as smoking and indulging in too much alcohol. Bad diets lead to high blood pressure and obesity. High blood pressure and high blood cholesterol are closely related to excessive consumption of fatty, sugary and salty foods. They become an even more lethal combination when combined with tobacco and excessive alcohol consumption. Be careful with having too much of a good life! It might become very short lived.
Cigarette smoking should be avoided by all and especially by patients following a stroke or TIA. Excessive alcohol should also be eliminated. Eating fruits and vegetables can help prevent cardiovascular diseases. Reduction of salt intake is an important message for the population at risk of a stroke. Salt reduction leads to reduction in high blood pressure and risk of stroke.
Physical inactivity causes about 15% of diabetes and heart disease. The American Heart Association recommends 30-60 minutes of exercise 3-4 times per week.
Walk, run, jog, exercise, play, dance, just do something! Stay alive.
Stroke is preventable and this article sets to tell you how. Dr. Ajayi (Federal Medical Center, Ido-Ekiti, Nigeria) found that patients who recognize their increased risk of stroke are more likely to engage in stroke prevention practices than those who do not. Perception about stroke among the 'at risk' population in the study indicates that more health education both at the community and the hospital is very vital to reducing the prevalence, recurrence, disability and mortality of stroke.
Knowledge is power. This is true and more so with stroke. The emphasis is on primary prevention and empowerment. We implore you to become an avid reader of stroke articles in newspapers, books and online. We beg you to discover a knowledgeable doctor or nurse who can help you unravel the medical mysteries and myths surrounding stroke. We beseech you to identify a doctor close to you who can provide effective and timely care for you when and if needed. Please discuss stroke with your local health provider and identify ways you can improve stroke care within your particular community. They should share accurate and current information on stroke care with you and empower you with tools to support you in your daily activities: to prevent you or your loved ones from having a stroke. Health providers are enjoined to communicate information about stroke risk to their patients.
October has been designated stroke awareness month by the World Stroke Organisation. We are using this forum to promote stroke awareness in Nigeria.
Learn about stroke. Teach someone else about stroke. Save lives.
Sunday 5 July 2009
transfacetal screw fixation for back pain

I have just returned from a trip to Austria to learn the technique of insertion of a transfacetal, transpedicular screw fixation for patients with severe back pain. The screw technique called PERPOS is interesting and has been applied for those patients (specially selected) who do not quite meet the criteria for pedicle screw fixation. This fuses the facets causing pain without interfering with the other joints. The procedure can also be reversed and converted to a pedicle screw fixation in the future if necessary. I like it. See the image above.
Friday 19 June 2009
Professor Ohaegbulam

It was a pleasure and an honour to meet the highly esteemed Professor Ohaegbulam in Enugu over the past few days. I travelled by air from Abuja to Enugu on a pleasant Friday morning to visit MEMFYS neurosurgical unit, in Enugu. This is the first private neurosurgical unit and perhaps one of the better equipped and functional neurosurgical units in the country.
I have not visited many neurounits in Nigeria but reports do suggest that many are struggling to provide adequate and qualitative service to the people. Indeed many units have a severe shortage of trained nursing staff, beds and equipment. This makes the job of the local neurosurgeon doubly difficult enabling Memfys to be well positioned in providing additional support for neurosurgical services in the country.
I had a wonderful time at the hospital and met many lovely people including of course, Mrs Ohaegbulam. I was shown round the hospital and was particularly suprised to see a CERETOM mobile CT scanner in the unit. I have obtained an internet image of the scanner for you to see. Its quite compact, functional with good image copies and can be battery powered. The unit is also planning to install an MRI scanner in the near future.
Prof mentioned about his speech on the state of neurosurgery in Nigeria. This is of interest to me as I am keen to write and rewrite the history for posterity. Such publications are therefore of real benefit. The Odeku Memorial Lecture published in the African Journal of Medical Sciences (Ibadan) on the practice of neurosurgery in Nigeria is a must read for all our neurosurgeons. Please see: Ohaegbulam SC: Half a Century of Neurosurgery in Nigeria. The 13th E. Latunde Odeku Memorial lecture. Afr.J.Med.Sci. (20098) 37,293-302. Unfortunately the copy is not available online but can be obtained direct from the publishers. Or get a friend to get the journal for you as I intend to do.
My visit to MEMFYS was a very memorable and enjoyable one. The professor found time in his very busy schedule to have quite insightful conversations with me. The range of topics was quite wide and I will share some with you in the next few weeks. I was truly honoured to be in his presence and will always remember the visit fondly.
Biodun Ogungbo
Image: The CereTom CT scanner
Sunday 31 May 2009
the ashanti graham health and education intiative foundation

Dr Douglas Okor recently donated a microscope and other equipment to the Department of Surgery University of Benin. This altruistic gesture which came to fruition under the auspices of the foundation is highly commendable. Its a small step in the right direction to assist in the development of neurosurgical services at UniBen. The picture shows Douglas (left) presenting a projector to the Head of Department. Dr Udor, neurosurgeon is seen in the background.
Tuesday 26 May 2009
case reviews
This blog is useful for discussions on interesting cases which could be learning points for us. If you have a case thats confounding or difficult you could share it here and hopefully get advice and opinion from someone who may have dealt with something similar. Pictures and videos can be loaded easily so makes it really worthwhile and a useful educational tool.
I will find a case I can share with you soon.
Biodun
I will find a case I can share with you soon.
Biodun
Saturday 16 May 2009
Recent publication from Nnewi
Hi there
This article below is one of the most enjoyable articles I have read recently. It relates to my earlier post and a start in the need to document the state of affairs in Neurosurgery. We do need to define where we are, the problems facing us and then we can form a pressure group to benchmark the changes required. This article is a welcome addition to the literature. Biodun
Neurosurgery in Nigeria--an evaluation of the perception of health personnel in a new centre and a comparison of the Nigerian situation with that of other African states.
Emejulu JK.
Department of Surgery, Nnamdi Azikiwe University & Nnamdi Azikiwe University Teaching Hospital Nnewi, Anambra State, Nigeria.
CONCLUSION: Neurosurgical service in Nigeria is grossly inadequate both in availability and quality, and these have resulted from bad government policies. It is therefore of utmost necessity that services and training be urgently provided in this specialty, at least in the tertiary institutions in Nigeria.
This article below is one of the most enjoyable articles I have read recently. It relates to my earlier post and a start in the need to document the state of affairs in Neurosurgery. We do need to define where we are, the problems facing us and then we can form a pressure group to benchmark the changes required. This article is a welcome addition to the literature. Biodun
Neurosurgery in Nigeria--an evaluation of the perception of health personnel in a new centre and a comparison of the Nigerian situation with that of other African states.
Emejulu JK.
Department of Surgery, Nnamdi Azikiwe University & Nnamdi Azikiwe University Teaching Hospital Nnewi, Anambra State, Nigeria.
CONCLUSION: Neurosurgical service in Nigeria is grossly inadequate both in availability and quality, and these have resulted from bad government policies. It is therefore of utmost necessity that services and training be urgently provided in this specialty, at least in the tertiary institutions in Nigeria.
Friday 15 May 2009
Nigerian Neurosurgeons
The leaders of the Nigerian Neurosurgical community that I know and have been in contact with are as listed below.
Professor Adeloye, Professor Arigbabu, Professor Shokunbi, Professor Ohaegbulam, Mr. Shehu, Malomo, etc etc.
However, there are without doubt many more practising all over the world: quietly contributing their quota in their local areas and internationally.
We need to start writing about the past, the present and the future of neurosurgery in Nigeria for posterity. This activity starts from a recognition of our elders, documentation of their contributions, and should lead to stimulating discussions and constructive engagement in documenting the history of Neurosurgery in Nigeria. There are now many more units in Nigeria and some are still in infancy. However, this is the time to start a chronicle of all the units and start collecting the names, pictures and record of achievements in each neurosurgical centre for the future. The young and the older neurosurgeons have a role to play. We are in a unique position to continue the excellent work done by our predecessors. We have to rise to the occasion and start another renaissance of Neurosurgery in Nigeria.
There are currently about 24 neurosurgeons practising in Nigeria and countless more working in other countries all over the world. What we need to do is link up and start real dialogue, social networking and educational programs to stimulate further development of Neurosurgery in Nigeria.
This I hope is a small beginning on this long long road.
Please email me details of Nigerian Neurosurgeons that you know so I can invite them to the blog. You can also invite them anyway and we can use this forum (restricted at the moment to neurosurgeons only) to communicate.
I will hopefully meet and document many more names as this blog develops.
Biodun
Professor Adeloye, Professor Arigbabu, Professor Shokunbi, Professor Ohaegbulam, Mr. Shehu, Malomo, etc etc.
However, there are without doubt many more practising all over the world: quietly contributing their quota in their local areas and internationally.
We need to start writing about the past, the present and the future of neurosurgery in Nigeria for posterity. This activity starts from a recognition of our elders, documentation of their contributions, and should lead to stimulating discussions and constructive engagement in documenting the history of Neurosurgery in Nigeria. There are now many more units in Nigeria and some are still in infancy. However, this is the time to start a chronicle of all the units and start collecting the names, pictures and record of achievements in each neurosurgical centre for the future. The young and the older neurosurgeons have a role to play. We are in a unique position to continue the excellent work done by our predecessors. We have to rise to the occasion and start another renaissance of Neurosurgery in Nigeria.
There are currently about 24 neurosurgeons practising in Nigeria and countless more working in other countries all over the world. What we need to do is link up and start real dialogue, social networking and educational programs to stimulate further development of Neurosurgery in Nigeria.
This I hope is a small beginning on this long long road.
Please email me details of Nigerian Neurosurgeons that you know so I can invite them to the blog. You can also invite them anyway and we can use this forum (restricted at the moment to neurosurgeons only) to communicate.
I will hopefully meet and document many more names as this blog develops.
Biodun
Subscribe to:
Posts (Atom)

